Monday, February 22nd, 2021
Comprehensive Maternal Health Coverage
By Eden Blackwell
Women need quality healthcare before, during, and after pregnancy for the best outcomes for moms and their babies. Through Medicaid, pregnant women with household incomes of up to 200% of the Federal Poverty Level (FPL) can gain access to health services during and a short time after pregnancy. But it doesn’t last, and gaps in coverage mean delays or missed care with possible repercussions for maternal and child health. Expanding Medicaid eligibility would increase continuous access to care for many low-income mothers before, during, and after a pregnancy. However, Medicaid-covered women with household incomes above expansion levels (138-200% FPL) would still be limited to sporadic access to care.
Gaps In Coverage Before, During, and After Pregnancy

Before
Twenty-five percent of Mississippi women surveyed within a year of their most recent birth reported not having health coverage in the month before becoming pregnant. Unless a woman is a parent or caregiver and earns less than 26% FPL (e.g., $475 a month for a family of three[i]), she does not qualify for Medicaid coverage until she becomes pregnant.
During
Under Medicaid coverage for pregnant women, access to care begins only after certification of pregnancy by a physician and approval by the Division Medicaid—typically a 45-day process. About 30% of Medicaid-covered women don’t have their first prenatal visit until after the first trimester[ii].
After
Medicaid coverage for pregnant women ends 60 days after delivery, but risk of illness and death related to pregnancy can continue up to a year after birth. Most (87%) of maternal deaths in Mississippi occur after delivery, many of them well after the end of coverage[iii].
Policy Options For Comprehensive Coverage
Several policies can address these gaps in care for women from households living at 138-200% FPL, including:
An extension of Medicaid coverage up to 12 months– The majority of preventable, pregnancy-related deaths occur after delivery, and pregnancy-related healthcare spending continues well into the year following a delivery, when many low-income women no longer have coverage[iv].
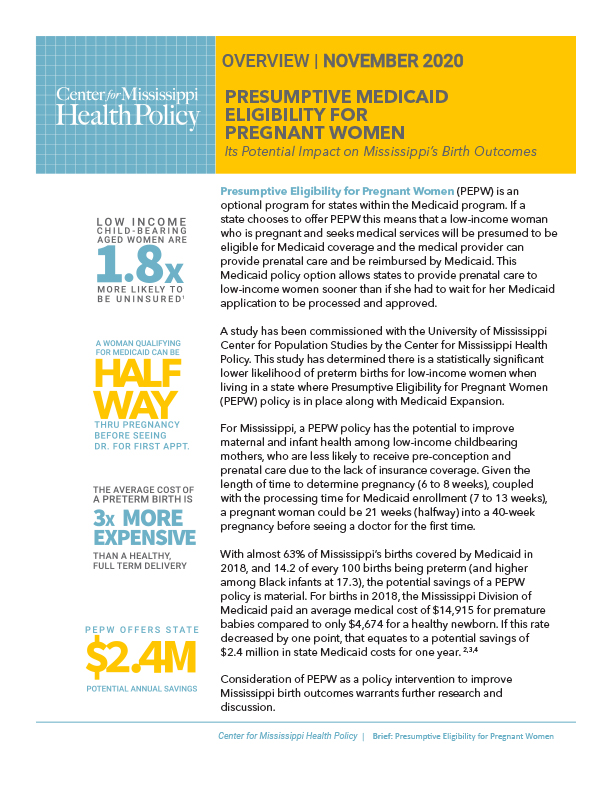
Presumptive eligibility for pregnant women– Twenty-nine states have policies that allow women to get timely prenatal care while the Medicaid approval process is ongoing. A recent review by Mississippi researchers has linked early access policies to improved outcomes for Black women and their children—a group with the highest risk of limited access to care and poor health outcomes[v].
Integration of non-medical health workers into pregnancy care- Community health workers, doulas, and midwives can support maternal care throughout pregnancy in ways that complement medical care and support good outcomes like full-term, vaginal deliveries and breastfeeding. Some states’ Medicaid programs currently pay or have explored paying for these support services.
Mississippi’s maternal mortality rate ranks 28th out of 51, and infant mortality in our state is the worst in the country, especially for Black babies[vi],[vii]. Cases of severe maternal illness also contribute to infant illness and death. Promoting the health of mothers supports the health of their children for years into their development. Medicaid covers at least 60% of births in our state and offers great potential to improve the lives of Mississippi families for generations through timely, comprehensive investments in women’s health.
To learn more about extending Medicaid coverage for postpartum women, read our latest issue brief.