A Survey of Mississippi Health Care Providers
For the print-friendly version, click here. | To download the report, click here.
Women in Mississippi experience high rates of unintended pregnancy, which can be associated with the use of less effective methods of contraception. In an effort to better understand the role of health care providers in contraceptive access, the Center for Mississippi Health Policy engaged researchers at the Social Science Research Center at Mississippi State University to survey medical doctors and nurse practitioners regarding their experience and opinions about the most effective family planning methods.
Women who seek family planning services at publicly-funded clinics in Mississippi are the least likely in the country to use the most effective reversible contraceptives. As health care providers are a key factor in a woman’s access to effective birth control, obstetrician-gynecologists (ob-gyn’s), family physicians, and nurse practitioners in Mississippi were recently surveyed about their knowledge, opinions and practice behaviors regarding long-acting reversible contraceptives (LARCs), the most effective, reversible methods of birth control.
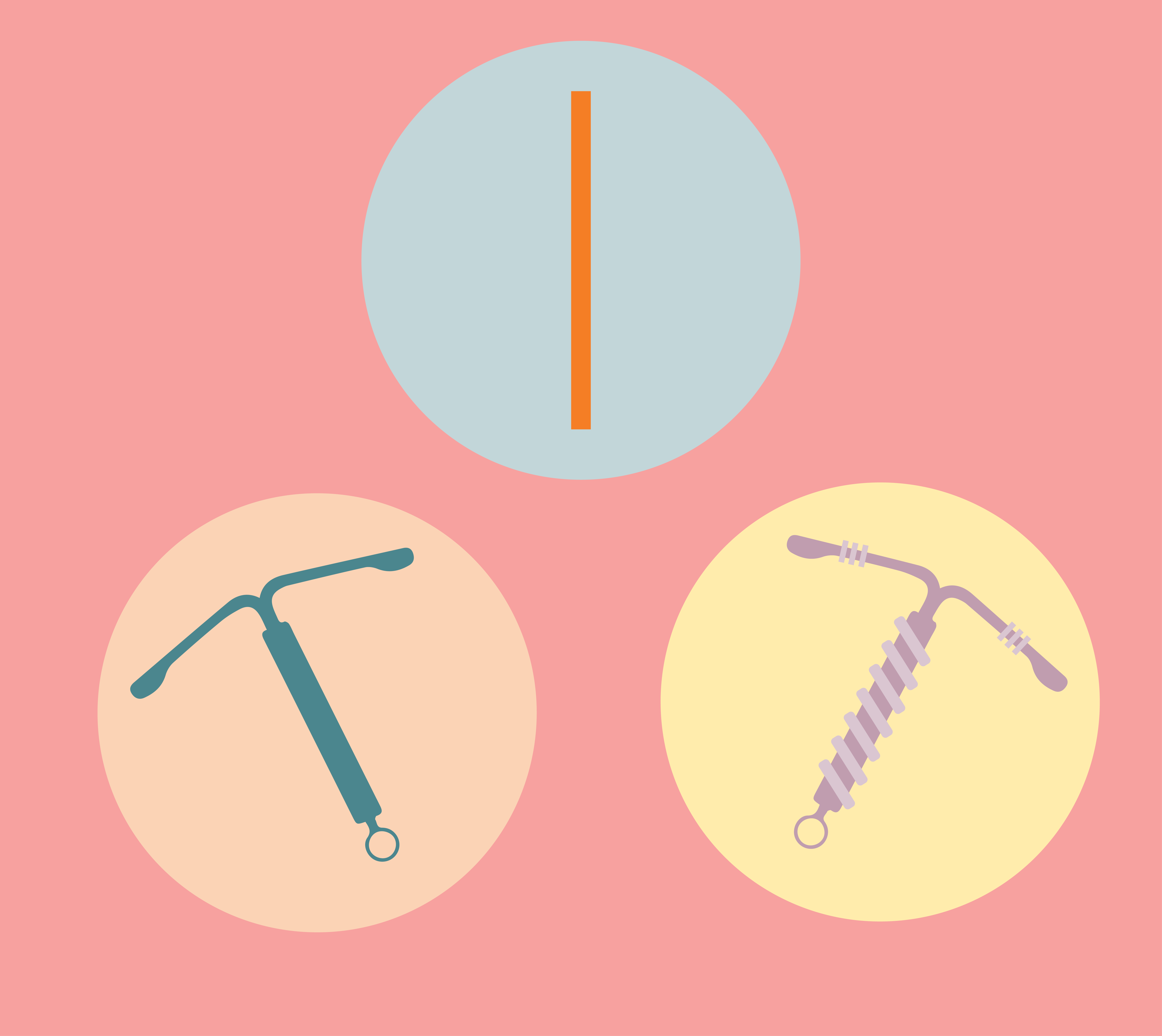
CONTRACEPTIVE METHODS BY EFFECTIVENESS
| Most Effective Reversible Methods* | Moderately Effective Methods: | Less Effective Methods: |
| Implant IUD | Injectable Contraception Vaginal Ring Contraceptive Patch Oral Pill Diaphragm | Male and Female Condoms Sponge Withdrawal Fertility-based Awareness Spermicide |
Source: Centers for Disease Control and Prevention. (2011).
More than 90 percent of ob-gyn’s included in this survey reported receiving training for counseling, insertion, and removal of LARCs, while just over half of family practice doctors and approximately 30 percent of nurse practitioners reported receiving training on LARC insertion and removal. As Figure 1 shows, ob-gyn’s report high numbers of insertions of LARCs, while family practice physicians and nurse practitioners are much more likely to refer women to other providers for insertions.
Nationally, 70 percent of women 18-44 rely on a family practice doctor as their regular source of care, while 14 percent rely on an ob-gyn, and 10 percent rely on a nurse practitioner. Each of these clinicians is trained to provide basic family planning and reproductive health services, however, ob-gyn’s, due to more specialized training, are more likely to provide the full complement of contraceptive options.
Factors Associated with LARC Provision
Because the providers most likely to be a woman’s regular source of primary and preventive care in Mississippi may be less likely to offer a full complement of family planning options, provider availability may be a key factor driving access to LARCs. Across the country, ob-gyn’s are in short supply and are projected to be in increasingly shorter supply as older physicians retire faster than newly trained doctors complete their training. This is especially true for Mississippi where the provider-to-patient ratio of 7.5 providers per 10,000 women ages 15-44 is one of the lowest rates in the United States.
Note
At time of publication, 5 medical doctors and 8 nurse practitioners serve all county health departments providing family planning services. Mississippi’s 20 FQHC grantees are staffed by 16 ob-gyn’s, 35 family practice physicians, and 180 nurse practitioners.
Despite a wide geographic distribution, few of these publicly-funded clinics provide ready access to the full range of contraceptive methods. Also, contraceptive services are not necessarily available on a regular basis and may have waiting periods for some services up to six weeks.
As of 2014, just 429 active ob-gyn’s served the state, practicing in just 36 of 82 counties and clustering in urban areas and around facilities with labor and delivery units. Women in the majority of counties in Mississippi face at least an hour-long drive for prenatal, delivery, and postpartum care, as well as family planning if they want to see an ob-gyn. Women without means to travel may be limited to publicly funded clinics which are less likely to be staffed by ob-gyn’s.
Provider training impacts patients’ use of birth control methods
Oral birth control pills are the most frequently used contraceptive method among patients of all providers responding to the survey (47 percent). Providers estimate that 15 percent use injectable hormonal contraception (Depo Provera), and 16 percent use LARCs (IUDs and Implants).
Family practice physicians and nurse practitioners, who are more readily available throughout the state and in rural areas, provide family planning and reproductive health services to many women; however many report a lack of training for LARC counseling or inserting and removing LARCs.
FIGURE 2. LARC TRAINING REPORTED BY PROVIDER TYPE
| OB-GYNS | Family Practice | Nurse Practitioners | |
| I have sufficient experience in inserting LARCs* | 97.3 | 29.0 | 22.0 |
| I have sufficient information to counsel patients about LARCs* | 100.0 | 80.0 | 68.5 |
| I was formally trained in LARC counseling* | 86.3 | 49.3 | 40.6 |
| I was formally trained in LARC insertion* | 97.3 | 54.8 | 29.2 |
| I was formally trained in LARC removal* | 94.5 | 53.4 | 32.4 |
| I have sufficient experience in removing LARCs* | 98.6 | 45.7 | 29.5 |
Medicaid medical claims data show that female beneficiaries 15-44 use moderately effective methods more than the most effective methods of birth control, but the degree differs by the type of provider rendering the service. Claims data for the period 2013-2017 show that twice as many patients of ob-gyn’s received LARCs as received Depo Provera injections. On the other hand, four times as many patients of family practice physicians, nurse practitioners, and other mid-level providers received Depo Provera injections as LARCs. (The oral pill is not included in this analysis due to industry billing practices.)
Provider Practice Patterns and Opinions
Provider opinion on the appropriateness of LARCs can vary for different patient populations. Figure 3 demonstrates the wide variation in reported provider opinion. Ob-gyn’s were more likely to recommend LARCs for patients regardless of age, number of sexual partners, or prior pregnancies.
ACOG COMMITTEE OPINION NO 10.
The American College of Obstetricians and Gynecologists has formally recommended that providers discuss LARCs with women of all reproductive ages including adolescents.
Health care providers are uniquely positioned to identify barriers to care within the health care system and, to some degree, within their patients’ lives. When asked about improving access to LARCs for their patient population, the top three areas for improvement suggested by all provider types were the following:
- Cost of care, including patient insurance coverage, out of pocket costs to patients, and low reimbursement for providers
- Patient education about contraceptives
- Access to contraception providers, including public clinics and trained clinician workforce
Practice conditions and LARC provision are strongly associated. Providers who perceived that conditions in their practice support offering LARC services reported higher numbers of actual LARC insertions in the past 12 months. Favorable practice conditions include the following:
- Acceptable reimbursement from private and public payors
- Adequate stock of LARC devices and reasonable cost to purchase them
- Sufficient staff and staff time to offer the service
Ob-gyn’s were significantly more likely to agree that their practice setting reflected these favorable conditions.
Summary
Providers with the most training and experience in LARC provision are in short supply and potentially out of reach for many women in our state. Data from a recent survey suggest that if a woman in Mississippi does not have access to an ob-gyn she is less likely to be able to access the most effective birth control methods if she wants them.
DELAWARE CONTRACEPTIVE ACCESS NOW (CAN)
Delaware, which had the highest unintended pregnancy rate in the country in 2010, recently focused on provider education and training on LARCs in publicly-funded clinics. Among Delaware Title X family planning clients aged 20 to 39, LARC use increased from 13.7 percent to 27.0 percent over 3 years.
COLORADO FAMILY PLANNING INITIATIVE
Colorado greatly increased the number of women using LARCs by reducing the cost of LARCs and providing patient education. That increase has been linked to a 35 percent decrease in abortion rates, a 40 percent decrease in babies born to teenage mothers, and a 12 percent decline in preterm births that occurred between 2009 and 2014.
MISSOURI CHOICE
The Missouri CHOICE project was able to support the uptake of more effective birth control among teenagers and young women through more comprehensive counseling on all methods of birth control. LARCs were the method of choice among 75 percent of participants.
Provider practice patterns based on attitudes, training, and understanding of LARC appropriateness have the potential to limit Mississippians’ access to family planning methods that could meaningfully impact their lives. Seventy percent of family practitioners and nurse practitioners (the most readily available provider types) have reported that they do not insert LARCs. Rather, those who recommend LARCs but do not insert the devices refer their patients to other provider types who do insert, but who may be long distances away.
Mississippi is unlikely to have ob-gyn’s locally available to all women across the state and in rural areas. However, a concerted effort will be needed to ensure that Mississippi women have access to providers offering all contraception services. Key components of such an effort include training non-ob-gyn clinicians on LARCs and educating patient populations about all contraceptive methods. These strategies can impact low utilization of LARCs and reduce unintended pregnancy rates as other states have shown.
Sources
- Lindberg, L., Santelli, J., & Desai, S. (2016). Understanding the decline in adolescent fertility in the United States, 2007-2012. Journal of Adolescent Health, 59(5):577-583.
- Center for Mississippi Health Policy. (2018). Preventing Unintended Pregnancy in Mississippi. http://www.mshealthpolicy.com/preventing-unintendedpregnancies/
- United States Department of Health and Human Services. Office of Population Affairs. (2017). Title X Family Planning Annual Report 2016 National Summary. https://www.hhs.gov/opa/sites/default/files/title-x-fpar-2016-national.pdf
- March of Dimes. (2015). 2015 Population of women 15-44 in Mississippi. https://www.marchofdimes.org/peristats/Peristats.aspx
- Pellegrine, I. & Southward, L. (2018). Long-Acting Reversible Contraceptives: Survey Results from Mississippi Health Care Providers. Social Science Research Center. Mississippi State University. Prepared for the Center for Mississippi Health Policy.
- Mississippi Division of Medicaid. (2018). Medicaid Medical Claims Data (2013-2017).
- Office of Mississippi Physician Workforce. UMMC. Distribution and Demographics of Mississippi Physician Workforce. (2014). https://public.tableau.com/profile/publish/Distributionand
DemographicsoftheMSPhysicianWorkforce/PhysicianWorkforce#!/publish-confirm - Health Resources and Services Administration. (2017). 2017 Health Center Program Grantee Data. https://bphc.hrsa.gov/uds/datacenter.aspx?q=d&year=2017&state=MS#glist
- American College of Obstetricians and Gynecologists. (2017). Committee Opinion No. 10. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Adolescent-Health-Care/Counseling-Adolescents-About-Contraception
- Birgisson, N.E., Zhao, Q., Secura, G.M., Madden, T., and Peipert, J. (2015). Preventing unintended pregnancy: The contraceptive CHOICE project in review. Journal of Women’s Health, 24(5), 349–353. http://doi.org/10.1089/jwh.2015.519
- Colorado Department of Public Health and Environment. (2017). Taking the Unintended Out of Pregnancy: Colorado’s Success with Long-Acting Reversible Contraception. https://www.colorado.gov/pacific/sites/default/files/PSD_TitleX3_CFPI-Report.pdf
- Welti, K. & Manlove, J. (2018). Unintended pregnancy in Delaware: Estimating change after the first two years of an intervention to increase contraceptive access. Child Trends. https://www.childtrends.org/wp-content/uploads/2018/03/UnintendedPregnancyDelaware_ChildTrends_March2018.pdf