The Mississippi Health Information Network (MSHIN) dissolved in 2019 after not being reauthorized by the State Legislature. To learn more about MSHIN while in operation please read below and to learn more about HIEs currently in operation visit SHIEC.
The shortfalls of documenting health care services in paper medical records were realized broadly after Hurricane Katrina hit the Gulf Coast in 2005. Mississippi has since enacted policies to promote electronic health information exchange (HIE). In 2010, the Mississippi Health Information Network (MSHIN) was authorized by law as the state entity to coordinate a statewide HIE. MS-HIN is up for reauthorization by state policymakers in 2019. This issue brief outlines MS-HIN’s progress and summarizes policy developments to inform the continued growth of the Network and the policy debates.
Mississippi Legislation
§41-119-1 ff
The Health Information Technology Act authorizes MS-HIN, provides its governance structure, sets the legal parameters for statewide health information exchange, and is up for reauthorization in 2019.
MS-HIN Designation
§41-119-3
“The Mississippi Health Information Network is a public-private partnership for the benefit of all of the citizens of this state.”
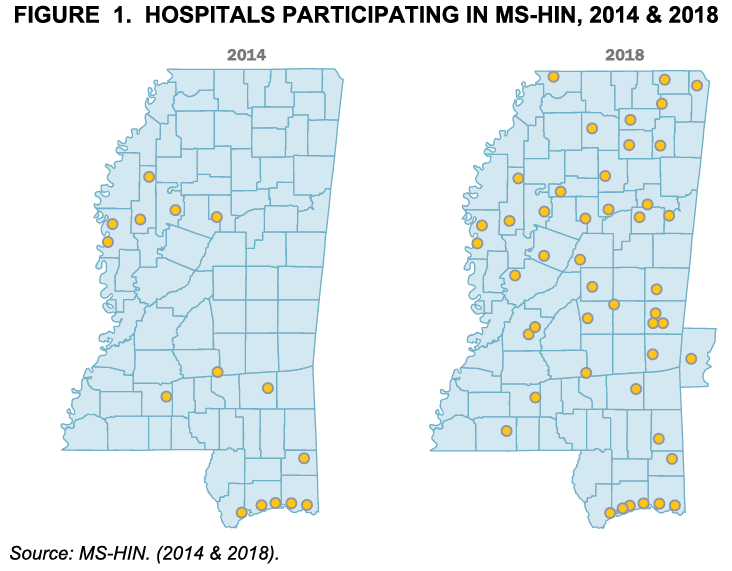
Figure 1 illustrates the growth of hospital participation in MS-HIN over time. Hospitals participating in the Network represent nearly two-thirds (61%) of all licensed acute hospital beds in the state. In addition to hospitals, over 800 clinics and other types of health organizations participate in MS-HIN.

Health Information Network (HIN)
Entity that provides the administrative structure
and manages the technology to facilitate health
information exchange among unaffiliated
organizations.
Health Information Exchange (HIE)
Process of sharing health information
electronically.
Interoperability
Ability of two or more systems or components to
exchange information and to use the information
that has been exchanged.
MS-HIN Operations
MS-HIN is an independent organization that serves a diverse set of stakeholders. It is governed by an 11-member board of directors who represent public and private health organizations (see sidebar). Administrative support for network operations is provided by the State Department of Health. Currently, MS-HIN participants electronically exchange laboratory, pharmacy, hospital, and clinical health information regardless of location. The available data are limited to those possessed by other providers participating in the network. The value of enrolling in MS-HIN is heightened as more providers participate and add their data. To date, most of the participating providers are hospitals and large health systems. Plans are in place to add reference laboratories, pharmacies, third-party payors, and other providers and organizations that are depicted in Figure 2.

How Does HIE Support Patient Care?
- Serves as an unbiased community data trustee for health information
- Connects health care systems, private HIEs, and independent providers
- Fills gaps in patient health information for more comprehensive patient records
- Provides real-time access to patient information for better clinical coordination and decisions
- Improves the quality, safety, efficiency, and reliability of care
MS-HIN Board of Directors
- Delta Health Alliance
- Health Insurance Carrier in MS (with IT knowledge, Governor appoints)
- Hospital in MS (with IT knowledge, Board of Health appoints)
- Information & Quality Healthcare
- MS Board of Information Technology
- Services (ITS)
- MS Department of Mental Health (Board of Mental Health appoints)
- MS Division of Medicaid
- MS Primary Health Care Association
- MS State Department of Health (Board of Health appoints)
- MS State Medical Association (a licensed physician)
- University of MS Medical Center
Health Data Reporting MS-HIN Can Support
- Cancer Registry
- Communicable Disease Surveillance
- Hospital Discharge Data
- Stroke/STEMI Registry
- Trauma Registry
Security & Privacy
MS-HIN provides secure health information exchange consistent with state and federal privacy and security laws.
MS-HIN Notify Service
Supports transitions of care by sending providers real-time notification when patients are admitted, released, or transferred from an emergency department or hospital so that they have timely information to manage their patients’ care.
While participation grew over the past decade, MS-HIN has not reached the critical mass necessary to be of enough value to some stakeholders. Participation is lacking by important partners, including some entities serving on its governing board. Currently, MS-HIN operates from participation fees and from State General Fund appropriations. MS-HIN fees are set by its board and have not changed since their adoption in 2011. In Fiscal Year (FY) 2018, 61 percent of the Network’s funding was generated by participation fees and the remainder came from State funds, nearly opposite from the ratio of its operational funds in FY 2015 (Figure 3).
Broader stakeholder participation is crucial to reaching sustainability by participant fees alone. Despite Network growth, ongoing challenges include rising vendor costs and limited staff. Raising stakeholder participation will bring more data into the Network and encourage others to participate. As MS-HIN brings increasing value to its participants, more providers will join the Network and pay participation fees. In return, additional resources will sustain and grow the Network.
Evolution of Health Information Networks
- Mississippi was among states that received federal funding over four years to help accelerate adoption of electronic health records (EHR) after the passage of the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act. In Mississippi, under the leadership of the Governor’s Health Information (HIT) Task Force, stakeholders used these funds to help build the legal and technical infrastructure that became MS-HIN. States had significant flexibility to develop HIEs that reflected their own existing infrastructures and organizational arrangements, and multiple models were developed. MS-HIN was one of a few state models assessed by researchers in 2014 to identify specific factors that promote or hinder implementation. Mississippi was noted for its following strengths:
- effective state privacy legislation;
- incentive program to promote provider enrollment; and
- requirements to use MS-HIN for certain public health reporting.
Studies of multiple HINs nationwide have identified some of the major barriers to building a successful exchange:
- lack of broad stakeholder engagement and financial participation;
- funds to continue development until user fees can sustain the network;
- few incentives for providers and vendors to participate;
- competition from other HIE efforts;
- absence of national standards;
- competitive business atmosphere that inhibits data exchange; and
- inability to integrate HIE into provider workflow.
Administrative & Policy Strategies
Strategies for alleviating these barriers vary widely state-to-state and differ between administrative and policy initiatives built on a range of governance models. Some strategies have spurred HIN evolution more so than others.
Governance Models
Some states have completely state-led governance models, others are structured with varying degrees of privatization, including Mississippi, and a few are solely private entities.
As MS-HIN revises its fee structure, it will need to strive to reach the best balance between generating sufficient revenue to sustain the Network and setting the fees at a level that is considered affordable by providers for the value received. MS-HIN is also in the process of adding new data sources (see sidebar) that will bring further value to participants. Arkansas has focused on refining integration in provider settings, with a goal of being the single point of entry to multiple systems. To address funding issues, Colorado worked with participants to simultaneously develop a sustainable fee structure and to build trust among participants by conducting stakeholder engagement meetings over several years.
Single Sign-On
Implements one set of log-in credentials (such as user name and password) to access multiple applications. MS-HIN is in the process of implementing this feature to streamline workflow.
Legislative initiatives can also help support HIEs. Eleven states mandate provider participation. North Carolina enacted legislation requiring hospitals to electronically submit select data on services paid by Medicaid to its HIN. Two states mandate public health reporting. Sixteen states offer financial incentives. Some subsidize costs of establishing connections to the state network or offer monetary rewards to those who use state HIN services. Indiana provided grants to some rural providers in exchange for HIE participation. Twelve states, including Mississippi, provide liability immunity to the HIE and participants.
Data Sources To Be Added Via New Grant Awards
- Behavioral Health
- Foster Care System
- Prescription Monitoring Program (PMP) Query
Summary
MS-HIN had a strong start, bolstered by outside funding that enabled the state to launch the effort with a sound structure and growth in initial participation. The Network has established itself as a proof of concept for interoperability. While MS-HIN has experienced increased funding from participation fees, it is not yet self-sustaining from those fees alone. For the Network to realize its potential, more health care providers need to participate. Provider participation is needed not only to supply revenue, but also to expand the volume of medical data available to its participating providers. Lack of seamless integration into provider workflow and incomplete stakeholder participation are barriers to the system reaching its full potential value. These barriers prevent the system from achieving a critical mass of statewide participation and threaten its path to financial sustainability.
To reach sustainability, increased participation can be driven through incentives, workflow support, mandates, marketing, or some mixture of these approaches. Multiple states have worked administratively to encourage participation by offering technical assistance, strategically structuring participation fees, and fostering dialogue with providers to build trust. Several states utilized legislative policy to address sustainability barriers. Some states mandated participation while others offered financial incentives such as waiving of certain fees in exchange for network participation. A few states provided grants to areas of need or to entities not otherwise able to afford to join the network. Every state HIN has different requirements and different needs, but state HINs strike a similar chord when implementing administrative and legislative policies to further the goals of creating efficiencies in data exchange and improving patient care.
Sources
- Adler-Milstein, J., Lin, S.C., & Jha, A.K. (2016). The number of health information exchange efforts is declining, leaving the viability of broad clinical data exchange uncertain. Health Affairs. 35(7): 1278-1285.
- Center for Mississippi Health Policy. (2018). Semi-structured key informant interviews of MS-HIN stakeholders, select officials in other state HIE offices, and the MS-HIN Board of Directors. Conducted June – September 2018.
- Dullabh, P., Parashuram, S., Hovey, L., Ubri, P., & Fischer, K. (2016). Evaluation of the state HIE cooperative agreement program final report. NORC at the University of Chicago. http://resource.nlm.nih.gov/101679172.
- Dullabh, P., Ubri, P., & Hovey, L. (2014). The State HIE program four years later: key findings on grantees’ experiences from a six-state review. NORC at the University of Chicago. https://www.healthit.gov/sites/default/files/CaseStudySynthesisGranteeExperienceFinal_121014.pdf.
- Fridsma, D. (2013). Interoperability vs health information exchange: setting the record straight. Health IT Buzz Blog. Office of the National Coordinator for Health Information Technology. https://www.healthit.gov/buzz-blog/meaningful-use/interoperability-health-information-exchange-setting-record-straight/.
- MS-HIN. (2018). An introduction to the Mississippi Health Information Exchange. Presentation to the Mississippi Primary Health Care Association (MPHCA), May 2018.
- Mississippi Code of 1972. (2014). Health Information Technology Act. §41-119-1–21.
- Office of the National Coordinator for Health Information Technology. (2018). A users guide to understanding the draft trusted exchange framework. https://www.healthit.gov/sites/default/files/draft-guide.pdf.
- Office of the National Coordinator for Health Information Technology. (2017). Connecting public health information systems and health information exchange organizations. https://www.healthit.gov/sites/default/files/FINAL_ONC_PH_HIE_090122017.pdf.
- Schmit, C.D., Wetter, S.A., & Kash, B.A. (2018). Falling short: how state laws can address health information exchange barriers and enablers. Journal of the American Medical Informatics Association.25(6): 635-644.
- Smith, P., Araya-Guerra, R., & Bublitz, C. et al. (2005). Missing clinical information during primary care visits. Journal of the American Medical Association. 293(5): 565-571.
- Strategic Health Information Exchange Collaborative. (2018). HIE 101. https://strategichie.com/resources/hie-101/#1519863086641-adb25ac0-rb35.
- 21st Century Cures Act, H.R. 34, 114th Congress. (2015-2016).